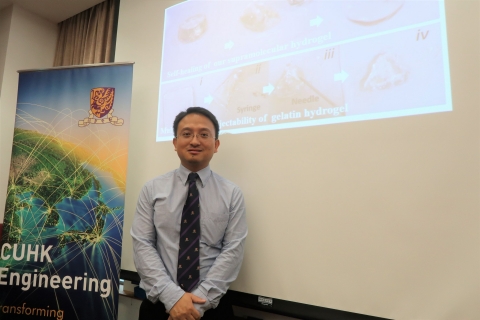
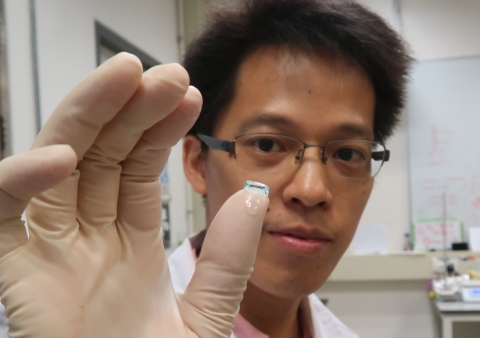
Prof. Bian Liming, Department of Biomedical Engineering, has recently developed a new class of injectable and slow-degrading hyaluronic acid (HA) hydrogels for osteoarthritis (OA). OA is characterized by the progressive degradation of articular cartilage in limb joints such as knees and hips, which can lead to significant pain and restricted mobility. A research team led by Professor Bian has proved that the HA hydrogels are ideal and affordable vehicles for delivering protein drugs and cells to assist treatments of human and animal arthritis, and a variety of other diseases including necrotic femoral head and intervertebral disc herniation. Athletes, workers and the elderly are highly susceptible to joint symptoms and degradation signs associated with defective cartilage and related changes in bone morphology. Patients with severe OA may have to use wheelchairs in some of the worst cases. Currently, a mild and common form of treatment is an injection of lubricants such as HA to soothe the joint pain. This is reported to be effective in temporary pain relief and in improving joint-motion in OA patients, through their lubricating and anti-flammatory properties. However, the existing HA solution degrades quickly and requires frequent injections for results that last from only six months to a year, causing a great deal of inconvenience and unnecessary expense for patients when the therapeutic effects gradually wear off. In terms of relief time, it is a big limitation for patients with severe degraded cartilage. Over the past two years, Professor Bian has been actively addressing this issue and making his research group one of the pioneers in transforming hydrogels innovatively. ‘The proposed hydrogels are injectable, slow-degrading and biopolymers-derived for clinical cartilage repair. In particular, they are very suitable for minimally invasive surgery as they can be tightly fitted into the irregular cartilage defects. The hydrogels can also promote recruitment of endogenous cells and be used for delivery of stem cells. They can even help load and control the release of small molecule drugs to enhance the performance on the affected area and reduce the atopic side effects at the same time,’ Professor Bian said. While the key to tackling OA is to strengthen the patients’ cartilage surface, the biopolymers-derived hydrogels play a key role. Not only do they have good bio-adhesion on cartilage, but the hydrogels demonstrate their resilient mechanical properties, high biocompatibility and self-healing capacity with the extracellular matrix (ECM). Professor Bian added that the safety and low cost will be a great advantage in transferring this technology. Funded by the Innovation and Technology Commission, his group is collaborating with the Prince of Wales Hospital and Shenzhen Second People's Hospital in clinical and veterinary cartilage repair on subjects such as racehorses and pets. He believes the application of the hydrogels will bring long-term benefit to more patients with varying joint problems in the near future.
|
|